In the realm of healthcare, innovation isn’t just about new drugs and treatments; it’s also about revolutionising the processes that bring these breakthroughs to the patients who need them most. One of the most transformative shifts in recent years is the integration of patient engagement into the regulatory approval processes for new treatments. This evolution is reshaping the landscape of drug development, significantly impacting timelines, and, most importantly, improving patient access to life-saving therapies.
The rise of patient engagement
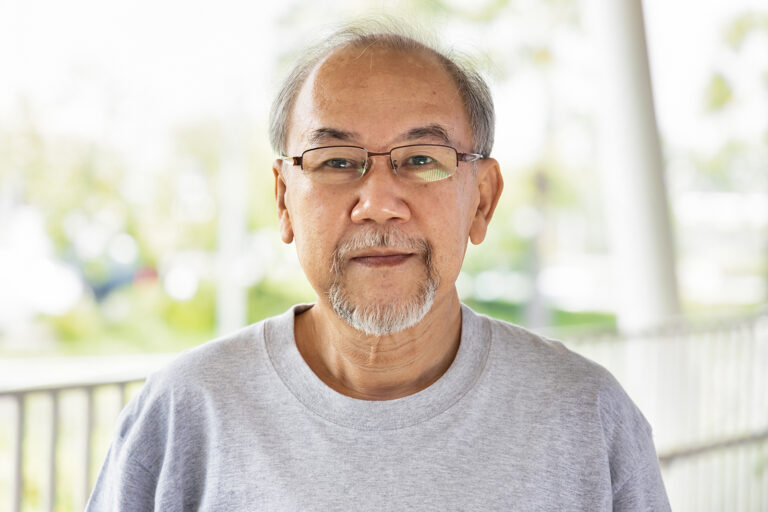
Traditionally, the development of new drugs was a process dominated by scientists, researchers, and regulatory bodies, with patients often relegated to the role of passive recipients. However, this dynamic is rapidly changing as patients are now being recognised as essential partners in the journey from laboratory bench to bedside. The inclusion of patient voices is not just a nod to ethics; it’s a strategic move that brings invaluable insights into the development process.
Patients have a unique perspective that is deeply rooted in their lived experiences with diseases and treatments. Their input can illuminate the nuances of symptom management, quality of life considerations, and practical challenges that may not be apparent to clinicians and researchers. This real-world insight is proving to be a game-changer in shaping more effective, patient-centric treatments.
The UK’s push for evidence of patient engagement in ethics submissions
The United Kingdom is at the forefront of integrating patient engagement into the regulatory framework, particularly in the realm of ethics submissions. In recent months, UK regulatory bodies and ethics committees have increasingly emphasized the necessity of patient co-creation in the development of new treatments. This progressive stance is transforming how pharmaceutical companies and research institutions approach drug development, ensuring that patient voices are not only heard but are instrumental in shaping the trajectory of new therapies.
Patient co-creation refers to the active involvement of patients in the research and development process, from the initial concept through to clinical trials and beyond. This collaborative approach ensures that the needs, preferences, and experiences of patients are central to the development of new treatments. In the UK, demonstrating evidence of such co-creation has become a pivotal requirement for gaining ethical approval for clinical trials and other research endeavours.
Ethical implications and requirements
The UK’s ethics guidelines now explicitly call for evidence of patient engagement in the design and implementation of clinical studies. This requirement stems from a growing recognition that patient input can significantly enhance the relevance and quality of research. Ethics committees are looking for concrete examples of how patients have contributed to:
- Study design and protocol development: Patients are involved in determining the research questions, study endpoints, and methodologies. Their insights help to ensure that the study addresses issues that are truly important to those affected by the condition being studied.
- Informed consent processes: Patient co-creation ensures that consent forms and procedures are clear, understandable, and genuinely informative. By incorporating patient feedback, researchers can create consent materials that are more comprehensible and meaningful to participants.
- Patient recruitment strategies: Patients can offer valuable advice on how to effectively recruit and retain study participants. Their involvement can lead to more inclusive and diverse study populations.
Impact on drug development timelines
One of the most profound impacts of integrating patient engagement into regulatory processes is the acceleration of drug development timelines. By involving patients early and throughout the development process, companies can identify potential issues sooner and adjust their strategies accordingly. This proactive approach helps to streamline clinical trials, making them more efficient and targeted.
For instance, patient feedback can lead to the design of more relevant clinical endpoints, reducing the likelihood of protocol amendments that can cause delays. Additionally, patient insights can help optimise recruitment and retention strategies for clinical trials, addressing common obstacles such as dropout rates and participant diversity. This can significantly reduce the time it takes to move from phase to phase in clinical trials, ultimately speeding up the journey to regulatory approval.
Moreover, regulatory bodies like the FDA and EMA are increasingly incorporating patient engagement into their evaluation processes. Programs like the FDA’s Patient-Focused Drug Development (PFDD) initiative are creating structured pathways for patient input, ensuring that the patient perspective is a key consideration in regulatory decision-making. This not only expedites the approval process but also increases the likelihood of approval for treatments that truly address patient needs.
Enhancing patient access
Beyond accelerating timelines, patient engagement is also enhancing patient access to new treatments. By aligning drug development more closely with patient needs and preferences, the resulting therapies are more likely to be effective and well-received. This leads to faster adoption and integration into clinical practice, ensuring that patients can benefit from new treatments sooner.
Furthermore, the shift towards patient-centric regulatory processes is fostering greater transparency and trust between patients, pharmaceutical companies, and regulatory bodies. Patients who feel heard and valued are more likely to participate in clinical trials, contribute to post-market surveillance, and advocate for broader access to new therapies. This creates a positive feedback loop that supports continuous improvement in drug development and approval processes.
The future of patient engagement
As we look to the future, the role of patient engagement in regulatory approval is set to expand even further. Advances in digital health technologies, such as patient-reported outcome measures (PROMs) and wearable health monitors, are providing new avenues for capturing patient insights in real-time. These tools are enhancing the granularity and immediacy of patient data, offering an unprecedented level of detail that can inform every stage of drug development and approval.
Additionally, the growing emphasis on personalised medicine is driving the need for more patient-specific data and input. Tailoring treatments to individual patient profiles requires a deep understanding of patient experiences and expectations, making patient engagement more critical than ever.The integration of patient engagement into regulatory approval processes is a revolutionary progression in the field of drug development. It is a change that promises not only to speed up the availability of new treatments but also to ensure that these treatments are more closely aligned with patient needs. As we continue to embrace this collaborative approach, we can look forward to a future where medical innovation is driven by the people it aims to serve, resulting in better outcomes, faster access, and a more compassionate healthcare system.