Implicit bias affects patient care and outcomes across a spectrum of underserved communities. Fact.
While this article focuses on the Muslim community, it’s important to note that implicit bias is a widespread issue, affecting various groups in unique and complex ways. By shedding light on these biases, particularly their impact on the Muslim community within the healthcare system, we aim to unravel the broader challenges and barriers that stem from these deep-rooted issues, hoping to pave the way toward a healthcare landscape characterised by understanding, empathy, and equity.
What is implicit bias?
Implicit bias in healthcare is like an unseen current, subtly guiding decisions and interactions in ways that are neither conspicuous nor fully conscious. These biases result from societal stereotypes and cultural conditioning that influence perceptions and actions without our explicit awareness. For example, a healthcare provider might unconsciously associate a patient’s ethnic background with certain health risks or lifestyle choices, potentially leading to diagnostic overshadowing or inappropriate treatment recommendations. This phenomenon is not just about individual attitudes but reflects broader systemic issues within healthcare education and practice that perpetuate these biases. To tackle implicit bias, it’s crucial to first acknowledge its pervasive presence and the many ways it manifests in patient care, from initial consultations to treatment plans and follow-up care.
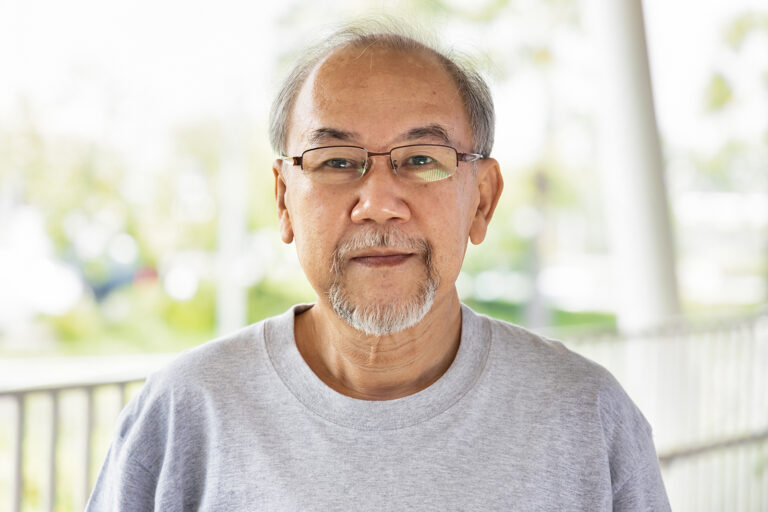
The experience of a Muslim family in the UK
The healthcare journey for many in the Muslim community is filled with barriers that go beyond the physical realm. Cultural misunderstandings, such as assumptions about language proficiency or religious practices, can significantly impede effective communication between healthcare providers and Muslim patients. For example, fasting during Ramadan is an essential aspect of Islamic practice that can affect medication schedules and nutritional needs. Yet, medical advice or treatment plans may not always consider it. This example highlights the nuanced challenges faced by Muslim patients, necessitating a more thoughtful, informed approach to healthcare that respects and accommodates cultural and religious sensibilities.
This personal narrative is from a friend of COUCH Health who recounts their grandmother’s recent hospitalisation due to an infection while also living with Alzheimer’s. This experience paints a stark picture of the impact of implicit bias on patient care. Despite the urgent nature of their grandmother’s condition, the family encountered a series of dismissive and prejudiced behaviours that exemplified the deep-rooted issues within the healthcare system.
- Neglected communication: The assumption that the patient’s family could not communicate in English led to significant oversight in care. This assumption not only delayed the necessary medical attention but also stripped the patient and her family of dignity and agency.
- Cultural insensitivity and stereotyping: Cultural sensitivity is the bedrock of compassionate healthcare, yet the family encountered scenarios that completely deviated from this principle. Firstly, halal food options were not available within the hospital—a fundamental dietary need rooted deeply in the Islamic faith. This not only dismissed the importance of accommodating religious practices but also signalled a lack of preparation and consideration for the diverse needs of patients. This was not a mere oversight; it indicated a larger issue where religious and cultural needs are often side-lined, inadvertently sending a message that certain patients’ requirements are secondary.
The insensitivity the family faced was further aggravated by a healthcare assistant’s deeply inappropriate comment, which insinuated that the responsibility for maintaining cleanliness fell on them because of their faith. This stereotype about Muslims being responsible for their own cleanliness in a medical setting is not only offensive but also completely contradicts hospital hygiene standards. Cleanliness in healthcare environments is a non-negotiable standard, critical for patient safety and care, and it is the duty of the hospital to ensure a hygienic environment for all patients, irrespective of their room’s privacy level. The lack of cleanliness in the patient’s personal bathroom and the subsequent refusal to address it promptly highlights severe negligence in maintaining a sterile environment—which is paramount in any healthcare setting. This incident is not just about a failure to clean a toilet; it’s a glaring reflection of systemic indifference to the patient’s dignity and the family’s rightful expectations of care. It undermines the very essence of healthcare, which is to provide care that is not only medical but also humane and respectful of all patients’ cultural and religious backgrounds. - Systemic exclusion: The disparity in treatment extended beyond the individual level, reflecting a systemic pattern of exclusion. The family were denied entry to the hospital under the pretext of visiting hours, while a white family was allowed entry at the same time, underscoring the racial and religious biases that influence the policies and practices within healthcare institutions.
- Challenges in clinical interaction: The lack of sensitivity was further exemplified when healthcare providers failed to acknowledge the father’s legal authority to make decisions on behalf of his mother, despite clear documentation. Three different white doctors questioned this legal authority before he was allowed to get on to the ward to talk to his mother. This not only caused unnecessary distress but also highlighted the systemic failure to recognise and accommodate the needs and rights of patients and their families.
- Impact on trust and healthcare engagement: These experiences have a long-term negative impact on trust in the healthcare system. The accumulation of microaggressions, cultural insensitivity, and systemic exclusion has not only affected their immediate healthcare experience but has also instilled a feeling of apprehension and mistrust towards healthcare institutions.
Let’s widen the lens of implicit bias
While the focus here is on the Muslim community, it’s imperative to understand that the challenges posed by implicit bias are not theirs alone. African American, Hispanic, Indigenous populations and LGBTQIA+ individuals frequently encounter similar biases that impact their healthcare experiences. For example, studies have shown that African American patients are often under-treated for pain compared to their white counterparts, a disparity rooted in historical prejudices and misconceptions. Similarly, transgender patients face significant barriers in accessing respectful and competent care, stemming from a lack of understanding and acceptance. These similarities across different communities underscore the systemic nature of implicit bias in healthcare, highlighting the need for a comprehensive, intersectional approach to address these issues effectively.
Clinical trials and mistrust
The underrepresentation of under-served communities in clinical trials is a critical issue, further compounded by historical injustices and current biases. This mistrust is not unfounded; past abuses in medical research have left deep scars. For the Muslim community, additional concerns arise from cultural and religious sensitivities that may not be adequately addressed or respected in the research context. The challenge lies in building trust and ensuring that clinical trials are accessible, culturally sensitive, and ethically conducted. Efforts to achieve this goal include community engagement initiatives, culturally tailored educational materials, and the inclusion of community representatives in research planning and execution. By addressing these barriers head-on, we can move toward a future where medical research is truly inclusive and reflective of the diverse populations it aims to serve.
Breaking down barriers
Addressing implicit bias requires a multifaceted approach encompassing education, policy reform, and cultural competency training. Healthcare institutions must prioritise diversity and inclusion at all levels, from the recruiting and training of healthcare professionals to developing policies and practices that actively combat bias. This includes integrating cultural safety into medical education curricula, providing ongoing training for healthcare providers, and implementing standardised protocols that minimise the influence of personal biases on patient care. Moreover, patient-centred care models that emphasise communication, respect, and partnership between patients and providers can significantly reduce the impact of implicit biases. These models encourage healthcare providers to see patients as individuals with unique backgrounds, experiences, and needs, fostering a more inclusive and equitable healthcare environment.
The journey toward dismantling implicit bias in healthcare is long and complex, but it’s a path we must navigate together. It calls for a collective effort among healthcare professionals, patients, policymakers, research organisations, and community leaders to foster a culture of inclusivity, respect, and empathy. By embracing diversity, committing to ongoing education, and advocating for systemic change, we can build a healthcare system that serves everyone with dignity and equity. Let this be our call to action: to work tirelessly in our respective roles to challenge and change the biases that undermine the health and well-being of underserved communities. Together, we can construct a new narrative in healthcare—one characterised by understanding, respect, and universal care.