Snapshot
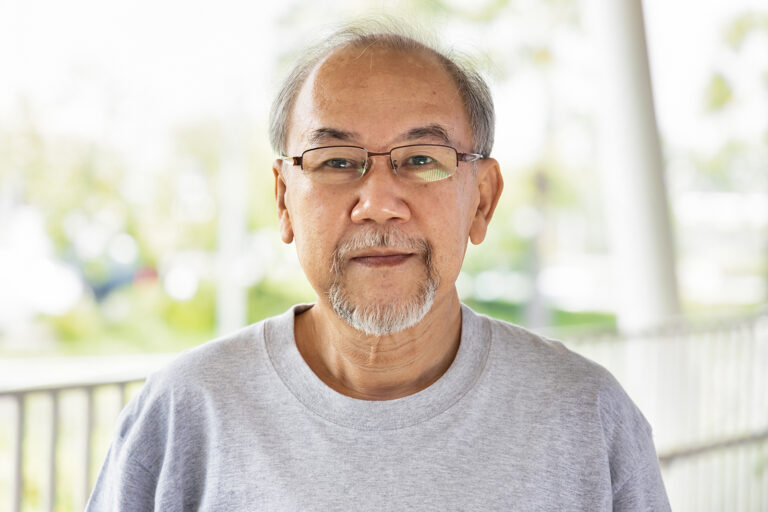
COUCH Health gained insights into the lived experiences of people with human immunodeficiency viruses (HIV) from Black, African American, and Hispanic communities in the US to ensure the design of HIV campaigns are representative, accessible and relevant.
Insights were gathered over 5 days using an anonymous online co-creation community platform, allowing participants to engage in daily discussions and complete tasks at their convenience.
From these insights, co-created campaign concepts and key considerations for future HIV patient-focused materials were developed to improve engagement with Black, African American, and Hispanic communities.
Problem
In the US, Black, African American, and Hispanic people have been historically underserved by healthcare and clinical research, despite being disproportionately affected by diseases such as HIV.
- Black, African American, and Hispanic people make up 70% of new HIV infections in the US
- African American women are 15 times more likely to die from HIV-related infections than White women
- Black women make up 54% of new HIV infections for women in the US, despite making up less than 15% of the population
- In the US, Black women accounted for 62% of HIV infections among Transgender women
- Only 8% of all PrEP* users in the US were female, despite making up 18% of new HIV diagnoses
*Pre-exposure prophylaxis (PrEP) is a preventative treatment strategy for individuals who are at risk of contracting HIV.
Racism, stigma, homophobia, poverty, and discrimination intersect to create significant barriers, resulting in inadequate access to preventative HIV measures and treatment. This contributes to widening disparities in HIV diagnoses and overall disease burden among underserved communities.
Strategy
COUCH Health facilitated an anonymous online co-creation community platform for people living with HIV from Black, African American, and Hispanic communities to share their insights.
The purpose of the online community was to:
- Gather feedback on campaign concepts for a HIV patient recruitment campaign
- Co-create culturally relevant patient-facing materials
Over 5 days, daily discussion topics and mood boards were released.
- Participants were able to contribute anonymously at their convenience and engage with other participant’s anonymised comments